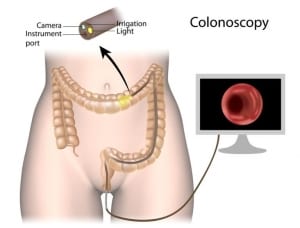
A colonoscopy is a procedure performed to visually examine the bowel. It is performed using a long, thin plastic tube with a light and camera at one end. The tube is flexible, allowing the Doctor to examine the inside the large intestine (colon) from all angles. The images from the camera are projected onto a screen for the Doctor to view. The tube is inserted into the rectum, under sedation so the patient does not feel anything. It is then manoeuvred through the colon to examine the health and appearance of the tissues that line the large intestine.
It is usually performed when a patient complains of one or more of the following symptoms, which have not been explained by other reasons:
- Blood in the stools
- Bleeding from the rectum
- Unexplained abdominal pain
- Changes in bowel habit, such as prolonged diarrhoea
- Pus or mucous in the stools
- Unexplained anaemia or reduced iron stores
The National Bowel Cancer Screening Program invites all people aged 50-74 years to participate in free faecal occult blood testing. If this test is found to be positive, colonoscopy may be recommended as a screening or surveillance test for colorectal cancer.
Colonoscopy is not routinely used for colorectal cancer screening in asymptomatic people but is suggested for those with a family history of colorectal cancer. A colonoscopy requires preparation. If you are on blood thinning medications, you may be required to stop these prior to the procedure. You will also need to discuss any other medicines, vitamins or supplements you are taking with your Doctor, prior to the procedure.
The procedure requires an empty, clean bowel in order to obtain quality views of the intestinal tissues. This usually involves taking a ‘bowel preparation’ substance that acts as a laxative to clean out any faecal matter. You will have to follow a protocol and your Doctor’s advice on what you can or cannot consume (food & beverage wise) leading up to the procedure. Sometimes, the doctor performing the colonoscopy may find polyps or other unusual looking tissues. The polyps and/or tissue may be removed or biopsied as part of the same procedure and sent to a lab for further investigation. Following a colonoscopy procedure, it is common to experience bloating, flatulence and mild cramping. Some light bleeding might occur if the Doctor has removed a polyp or tissue sample.
Other post-procedure symptoms such as excessive bleeding, fever, chills, severe abdominal pain, severe bloating, persistent nausea & vomiting, excessive thirst, dizziness and/or headaches are NOT normal following a colonoscopy and should be discussed with a Doctor immediately. A colonoscopy is a day procedure and you will be able to go home a few hours afterwards. You will be instructed NOT to drive for 24 hours following your procedure, due to the effects of the anaesthetic.
Most of the time, a colonoscopy is very straight forward and there are no complications. In about 1 in 1000 cases, the scope may cause a perforation in the bowel wall, which requires surgical intervention. Based on recent statistics obtained from the National Bowel Cancer Registry, four out of ten people who have a colonoscopy will have a clear result. Around half will be found to have a polyp; and one in ten is found to have a cancerous growth. If the cancer is found early, chances of a full recovery are very high. If your colonoscopy is clear, that is, no polyps or other cancerous growths are found, it indicates a low likelihood of colorectal cancer developing in the next 10 years. Your Doctor may recommend a surveillance colonoscopy in 5 years if there is a clinical indication or family history.